Through improved care coordination, patient outreach and engagement, the HP2 Clinically Integrated Network— which includes providers from Northeast Georgia Health Partners — advanced a population health initiative focused on empowering diabetic patients to improve their health outcomes.
Summary
If not effectively managed, patients with diabetes can experience serious health risks. Diabetes can also be costly to the patient. To positively influence these outcomes, a population health initiative focused on empowering diabetic patients has helped patients improve their health through effective diabetes management.
Population Health objectives for our diabetic patients focus on the following:
- Improving the care coordination process between different provider teams.
- Being proactive with education and outreach, including early outreach for those newly diagnosed.
- Supporting patients to adopt steps to better manage their condition, including measuring blood glucose levels at home, keeping medical appointments, making recommended lifestyle choices, receiving recommended screenings, and taking advantage of other opportunities to improve health, such as attending nutrition classes.
- Maintaining healthy A1C levels.
What is population health, and why is it important?
Population health is an approach to care that promotes collaboration among all services and service providers (hospitals, physicians, community groups, etc.) that work together to deliver improved outcomes in their communities. These partnerships work across the continuum of care, providing solutions to ensure people have seamless access to the right care, at the right time, at the right place, and – ideally – at the right cost.
Population health delivery has become increasingly important as more health systems and providers seek better ways to improve the health of the people in their communities. Population health encourages Providers to focus on preventative measures, interventions, and incentives to promote health and wellness throughout the community.
Population health initiatives throughout northeast Georgia
In support of its population health initiatives, Northeast Georgia Health System (NGHS) — a not-for-profit community health system serving Northeast Georgia — participates in the Northeast Georgia Health Partners Network. Health Partners is a wholly owned subsidiary of NGHS that brings regional physicians and hospitals together as a preferred provider organization (PPO) to serve managed care plans. Health Partners also created HP2, a physician-led, Clinically Integrated Network (CIN) that includes physicians and advanced practitioners from Northeast Georgia Medical Center, Longstreet Clinic, Georgia Heart Institute, Northeast Georgia Physicians Group, and other independent practices in the north Georgia area.
CINs are increasingly popular as providers seek to collaborate with like-minded healthcare partners such as hospitals, physician groups and others to improve access to and quality of care, streamline care to reduce unnecessary services and treatments, and reduce avoidable hospital admissions and visits to the ER.
Background
Diabetes is an epidemic in the United States (American Diabetes Association, 2021). The Centers for Disease Control and Prevention (CDC) estimates that more than 37 million Americans are living with diabetes, and another 96 million are prediabetic (CDC, 2022). Approximately 90-95% of those living with diabetes have Type 2 diabetes which most often develops in adults over the age of 45, although it is becoming more prevalent among younger people (CDC, 2021). The number of adults diagnosed with diabetes has more than doubled in the last 20 years, and it’s the seventh leading cause of death in the United States (CDC, 2022).
Diabetes poses health risks such as heart disease, stroke, amputation, end-stage kidney disease, blindness and death. In addition to serious health complications, diabetes is costly. In Georgia, more than 12% of the adult population is living with diabetes, costing an estimated $11 billion annually (American Diabetes Association, 2021).
Managing Diabetes
Diabetes management requires strong self-discipline on the part of the patient in that they take many recommended steps, including making healthy lifestyle choices, getting various regular screenings, and actively monitoring blood glucose levels. The most important person who can manage diabetes effectively is the person living with diabetes, but this can be challenging, especially for patients who lack the support, knowledge, and resources that are important for diabetes management.
Providers’ lack of streamlined care coordination also poses risks for diabetic patients. Dr. Linu Joseph is a Northeast Georgia Physicians Group family physician and a provider in the HP2 network, and more than 50% of her patients are living with Type 2 diabetes. She says that it’s important for patients to be proactive in their care, but the reality is that they need help from providers when it comes to reminders and care coordination.
“Part of it is education—patients need to know why they need to do certain things every year, but they also need to be reminded,” she said.
When patients don’t follow recommended screenings or appointments, they are more likely to become reactive in their care—seeing the doctor when they have a health problem that might have been avoided with recommended preventative services or appointments. This can lead to avoidable—and extremely costly—appointments or, worse, trips to the ER. A lack of coordinated care also means patients receive unnecessary or duplicative services. Patients may also face challenges when navigating insurance coverage issues, with some diabetes medications being covered by certain insurance providers while others are not.
Dr. Joseph says a common barrier to diabetes management is the misconception that patients can manage their diabetes with lifestyle choices alone.
“I think a lot of people are hesitant to take medications because they think they failed. That’s one of the biggest challenges I see, especially with younger patients in their 40s and 50s. I see a lot of shame or embarrassment. They feel like if they eat right, they should be able to manage it, but that’s a misconception because that’s not how your body works. It takes a lot of time and effort to educate them on what diabetes is and about insulin resistance.”
Alternatively, Dr. Joseph says that the other most common misconception she sees is that patients think medications alone will work.
“We also see the opposite where people think that since they are taking medication, they can eat whatever they want.”
Another challenge to effective diabetes management is that patients are typically struggling with other health issues that need to be treated, such as obesity or other chronic conditions. Additionally, Dr. Joseph says that many of her patients are also dealing with mental health disorders which may be exacerbated by—or contributing to—their diabetes diagnosis.
“When their depression gets worse, their diabetes gets worse,” she said.
There are a lot of things to consider with a diabetes diagnosis and Dr. Joseph says that to be effective, she must look at a patient’s health holistically.
“I’m not just treating diabetes; I’m treating the whole person.”
Opportunities to Improve Diabetes Management
HP2 aims to work with its providers to make diabetes management easier for patients. HP2 identified areas to streamline and improve care delivery processes, such as opportunities to educate and empower patients to embrace steps to improve their health.
Maximize and Streamline Data to Improve Care Coordination
The work of HP2’s Clinical Quality Committee supports improvement efforts by regularly reviewing patient data to identify and close care gaps. For diabetic patients, they look at indicators such as when patients are due to have their A1C levels checked, which is assessed with a simple blood test that reflects the risk of developing diabetes complications (American Diabetes Association). Other indicators might include the last time patients had a recommended diabetic eye exam, their lipid levels checked, or their feet examined. HP2 sends this information to clinical quality teams that work for providers within the HP2 network. In recent years there has been a concerted effort for providers to consistently track patient data using the same medical record system called Epic. With Epic, multiple providers involved in someone’s care can access the same patient information, which allows them to identify more easily—and address—care gaps.
Dr. Joseph says that a centralized database allows providers to see a complete picture of someone’s health, and they can use each point of care opportunity to encourage patients to follow up on recommended appointments or screenings.
“Every visit, we close the gaps as much as we can. Even if they’re not there for a diabetes-related appointment, but we can see that they, for example, are due for an A1C screening, we’ll ask if we can screen them right then.”
Additionally, HP2 recently began using care managers to help with care coordination for patients with chronic conditions like diabetes. For example, if a patient has been in the hospital for complications due to diabetes, a care manager will reach out to the patient after they’ve been discharged to check on them and ensure they understand their discharge instructions and review recommended next steps. If a patient has multiple chronic conditions, the care manager may encourage them to enroll in a special program where they regularly check in with a nurse who will conduct health assessments.
Patient Engagement and Education
Armed with more accurate data, quality team members from provider offices conduct education and outreach with diabetic patients, and they tailor the outreach based on patient needs. For example, a patient who has a history of high A1C levels may require more engagement—and more frequent appointments—than a patient whose A1C levels stay within the recommended range.
Though a feature in Epic called MyChart has made it easier for patients to interact with their doctors electronically through a messaging function, Dr. Joseph says a phone call or face-to-face interaction is usually more effective.
“We’ve found that human outreach works better.”
Engagement is also important when educating diabetic patients about regularly checking their blood glucose levels and helping them find a medication that works best for them. Dr. Joseph says that it’s important to let patients know that if they experience side effects on one medication, there are other options.
“I don’t want them to get discouraged if they have a negative side effect,” she said. “I think it puts them at ease when I’m able to give them more options.”
Dr. Joseph says she’s fortunate to have a pharmacist and pharmacy technician on her team who not only help patients find the right medication and adhere to it but also help them navigate potential insurance challenges, so they have access to the best medication.
Educating patients on the importance of taking their prescribed medication is key in helping them effectively manage diabetes, and so is encouraging patients to make recommended lifestyle choices like proper nutrition and exercise. Most patients have access to education classes through their insurance companies or their provider, and Dr. Joseph will encourage them to take advantage of all available resources.
Though patients with more complex issues may eventually need to be referred to an endocrinologist, Dr. Joseph says they do everything they can to manage a patient’s diabetes without referring them to a specialist. It typically takes months to get an appointment with an endocrinologist and based on where these specialists are located, access can pose challenges for some diabetic patients.
“We try our very best to keep them in our practice. Having a pharmacist and pharmacy tech on board helps get them the right medications,” she said. “We can also do insulin pumps and continuous glucose monitoring, which were traditionally done by an endocrinologist. We have more resources now, and we’re able to do a lot more than we used to.”
Engagement is equally important in helping patients before they get diabetes. Concerted efforts are in place to educate patients who are prediabetic or at high risk of developing diabetes.
“Primary prevention is our job,” Dr. Joseph said. “We also try to focus on those who are prediabetic to make sure they are on a healthy diet and know the importance of physical activity. We want them to know how important it is to prevent diabetes.”
Results
As a result of HP2’s diabetes management population health initiative, providers within the HP2 network have helped diabetic patients better manage their diabetes, as measured by their A1C levels.
Maintaining an AIC of less than 7% is the goal for most adults with diabetes (American Diabetes Association). An AIC greater than 9% indicates poor control of diabetes (Medicaid.gov, 2022). The figures below are provided by the Centers for Medicare and Medicaid Services and are from a sampling of Medicare Beneficiaries within the HP2 network who are diabetic. They represent the percentage of the patient sample who have an AIC equal to or higher than 9%. A lower percentage is better, as it reflects fewer diabetic patients who are considered to have poor control over their diabetes.
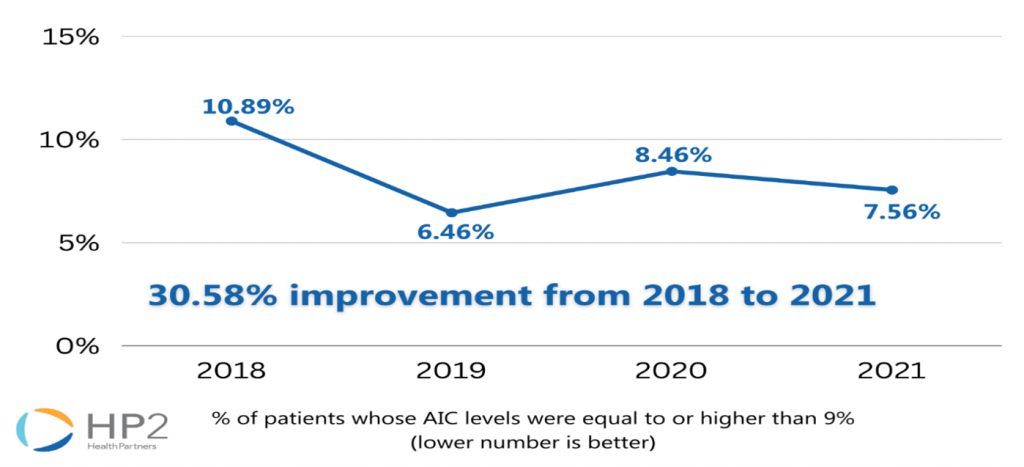
From 2018 to 2021, there was a 30.58% improvement in patients’ AIC levels in the Medicare Shared Savings Program Accountable Care Organization.
Next Steps
Endocrinologist Recruitment
Several efforts are underway to continue helping patients better manage their diabetes. For example, Longstreet Clinic—a primary care and multi-specialty medical group that operates several locations in Northeast Georgia—recently hired an endocrinologist to its team, expanding access for patients with more complex needs because of their diabetes. More providers are seeking to recruit endocrinologists. Equally important, more education and research is available to help primary care providers better support their diabetic patients and know when it’s time to refer them to an endocrinologist.
Technology
There are also increasing efforts to promote easy-to-use technology such as Continuous Glucose Monitoring (CGM), which are devices that allow patients to monitor their glucose levels continuously, and then easily share results with their providers. Additionally, research is underway for developing text-messaging-based applications that are integrated with monitoring devices to allow a patient and provider to easily communicate via text, for example, when issues arise, such as a provider texting a patient when they see a spike in their patient’s glucose level.
Communication and Coordination
Providers will continue to look at ways to use and share data to identify more patients at risk of developing diabetes or who may already have diabetes but have not yet been diagnosed. Processes will continue to evolve, promoting improved communication and coordination among providers and specialists with the ultimate goal of providing high-quality care tailored to each patient’s needs.
Patient Empowerment
As population health evolves, providers will continue to focus on ways to make it easier for their patients to maintain and improve their health. More and more community-based programs and resources are being developed—in partnership with health systems and providers—giving people easy access to free resources and information that empower them to take control of their health and well-being.
Summary
While HP2 has significantly improved outcomes for the diabetic population, continuous improvement is a journey. We are committed to positively influencing the lives of our patients through better care and health.
References
American Diabetes Association. (2021, October). The Burden of Diabetes in Georgia. Retrieved from ADA: https://diabetes.org/sites/default/files/2021-10/ADV_2021_State_Fact_sheets_Georgia.pdf
American Diabetes Association. (n.d.). Understanding AIC. Retrieved from ADA: https://diabetes.org/diabetes/a1c
CDC. (2021, December 16). Type 2 Diabetes. Retrieved from CDC: https://www.cdc.gov/diabetes/basics/type2.html
CDC. (2022, January 1). Diabetes Basics. Retrieved from CDC: https://www.cdc.gov/diabetes/basics/index.html
Joseph, L. C. (2022, June). Family Physician, Northeast Georgia Physicians Group.
Medicaid.gov. (2022). Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%): Ages 18 to 75. Retrieved from Medicaid.gov: https://www.medicaid.gov/state-overviews/scorecard/comprehensive-diabetes-care/index.html
